How Innovators are Advancing Health Equity for Medicaid Members

As 2023 rolls in, health plans are all talking about advancing health equity, especially in the Medicaid arena. One of the most common causes of health inequities is inadequate access to care. So, how are innovative health plan leaders going about improving access to reduce health care disparities for Medicaid members?
More Robust Provider Directories
Many plans are providing better directories of the providers who have contracted with the plan. What do we mean by better? It’s not just about clean data (although that’s part of it, and part of the service ReferWell provides). Better means including in provider directories searchable information that supports equitable care — such as the languages spoken in provider practices.
This Kaiser Family Foundation article states that individuals with limited English proficiency make up a disproportionate share of the Medicaid population and face challenges as a result. When health plans make it easier for members to communicate with doctors in their preferred language, members understand their care plans and have better outcomes.
Defining Care to Include More Than Just Visits to the Doctor
More and more Medicaid plans are including coverage for accessing an array of non-medical services (so-called Social Determinants of Health or SDoH agencies) to help members address needs like food insecurity, transportation to/from doctor visits, housing insecurity and the like.
But what good is providing broader access if the onus for accessing it continues to fall on the patient? Adding to the list of places that members can seek out, try to reach, wade through the “auto-attendant from hell” and then be put on hold interminably doesn’t really feel like a solution that is addressing health equity to me.
A few plans are taking the innovation a step further and not simply covering those social services. Innovative plans are meeting the members where they are by helping with SDoH referrals and appointment scheduling. Some plans use care navigators who reach out to beneficiaries to schedule visits to providers and SDoH agencies; others enable providers to book referral appointments with community-based organizations right at the point of care. For those plans that go the route of care navigators, there is an opportunity to also educate the member on the vital importance of a particular preventive care screening for which he or she may be overdue, such as breast cancer screening or colonoscopy.
Taking the burden off the member vastly improves not only the member’s experience but also their opinion of how much their plan cares about access to care and health equity. Besides being key areas of the CAHPS survey that determines part of the plan’s state quality ratings (or Stars in the case of Medicare Advantage plans), these innovations help get more members to the care they need, with subsequent improvement in their health outcomes.
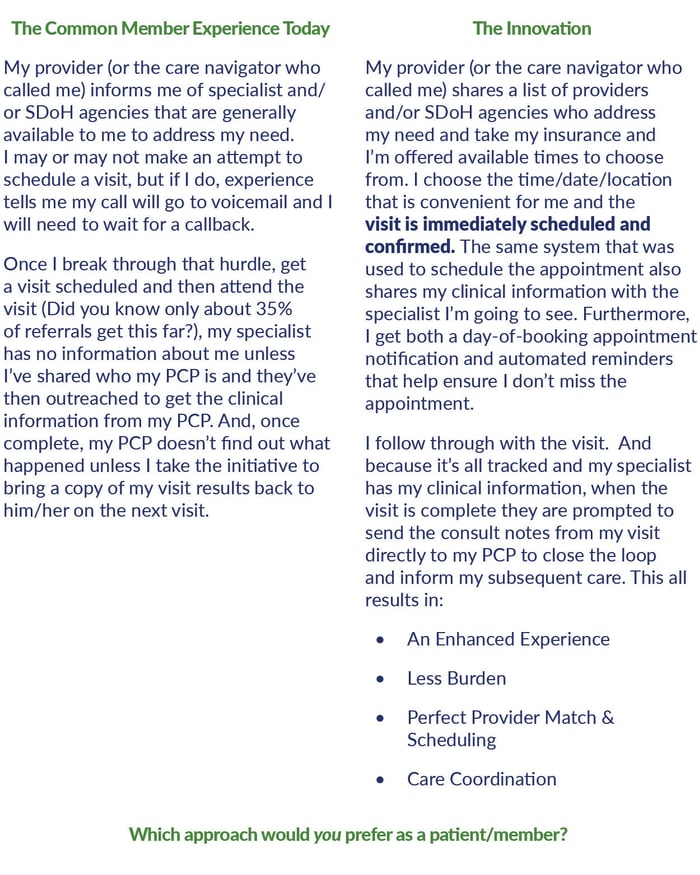
This is a simple innovation, but a powerful one with numerous benefits to the plan and the member:
- Simpler, easier access to care improves members’ perception of the plan and increases reported satisfaction in key CAHPS measures.
- Referring members to in-network providers who meet their social needs and have shorter wait times increases the members’ show rates, reduces out of network visits, and reduces the time to appointment by as much as 30%.
- Getting more members to receive the care they need, whether from a provider or an SDoH agency, reduces avoidable ER visits and reduces the total cost of care for those patients.
- All of the above improve HEDIS measures that increase the quality scores and thereby raise plan revenues at the same time as they reduce costs.
- Streamlining the care coordination and communication between providers improves their satisfaction with the plan and leads to increased engagement.
Which kind of innovator do you (or does your plan) want to be?
Written by Vytas Kisielius
Vytas has a long career building successful companies in many different capacities across the financial, IT and healthcare sectors. As ReferWell’s CEO, he works tirelessly to ensure ReferWell thrives within the market. Vytas draws on his extensive experience in creating a cohesive, hard working team while building and executing a focused strategy aimed at leading the way in revolutionizing healthcare delivery.
 © COPYRIGHT REFERWELL
© COPYRIGHT REFERWELL 