Boost Your Plan’s CAHPS Scores with Efficient Appointment Scheduling and Care Coordination

The most recent guidance from the Centers for Medicare & Medicaid Services includes some significant changes to Consumer Assessment of Healthcare Providers and Systems (CAHPS) scoring for Medicare Advantage plans.
While this year’s surveys were already sent to members and being processed, you should already be thinking about how you can close more care and improve your members’ experiences to influence next year’s surveys. You’ll be happy you did, when next year’s Star ratings come out.
The following image shows how several measures — including getting needed care, getting appointments and care quickly and care coordination — have quadrupled in weight on the CAHPS surveys distributed to plan members.
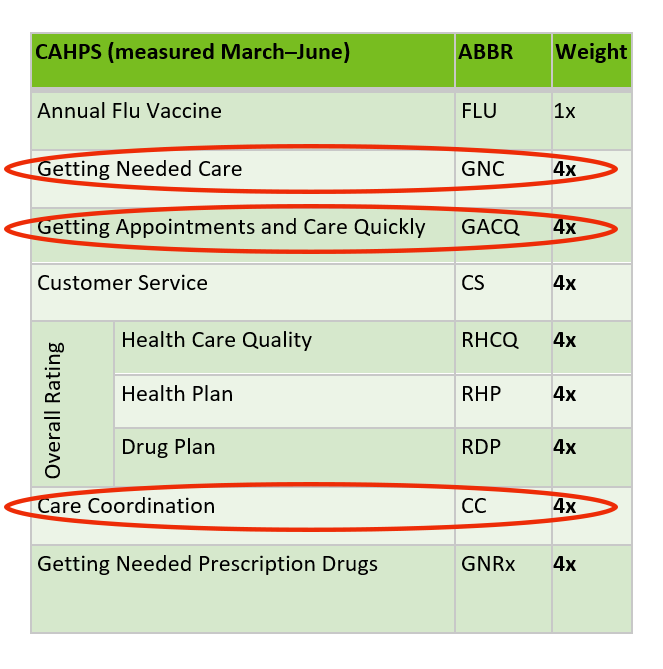
With CAHPS making up 32% of a plan’s Star rating, you can’t afford to overlook how you’re getting patients the care they need, quickly and efficiently, and providing appropriate follow up care.
Let’s take a deeper dive into the impact of these measures and how improving payers’ appointment scheduling and care coordination processes can increase member ratings in three of the heavily weighted areas of CAHPS.
CAHPS Measure: Getting Needed Care
Accessing and scheduling care can be challenging for members. Too often, the burden of finding care falls on the member, but there are several areas where payers and providers can work together to simplify the process of connecting members with the care they need:
- Provider Data Accuracy — It is estimated that half of insurance provider directory records are inaccurate. That not only leads to a frustrating member experience, but also causes members to give up and skip necessary care altogether.
Action Item #1: Commit to cleansing your provider database regularly so that members have the most up to date information on providers’ insurance accepted and practice locations.
- Provider Selection — Members look to their health plans for help choosing a PCP and look to both their plans and PCPs for support selecting a specialist that meets their needs. How are you supporting members with choosing a provider, so they are more likely to seek care?
Action Item #2: Use a tool that filters providers based on member needs and prioritizes the plan’s highest quality, lowest cost, most convenient in-network doctors. That way, members visit the optimal provider as defined by the plan; there are no unexpected bills for the member and plans keep the cost per member down.
- Access to Care — Often, there is a simple lack of specialists who can treat a member for his or her need. Factors including case complexity — as well as social factors such as language spoken and availability of transportation — are barriers to the member getting needed care.
Action Item #3: Prioritize clear insight into your network adequacy. Ensure you have enough specialists to send members to, that they have all the right equipment and services available, and that they can support the member’s preference for in-person or virtual visits.
- Member Follow Through with Appointments — By some estimates, up to 50% of all recommended specialty referrals never happen. Much of that is because plans and providers have long and inefficient processes for scheduling referral visits, and largely put the onus of the effort on the member.
Action Item #4: Help members book specialist appointments while still in the PCP’s office (at the point of care), or book annual wellness visits and care gap appointments on the phone with a care navigator on behalf of the plan (at the point of call). Doing so leads to patients showing up for those appointments 60% more often (for Medicare and Commercial members) and more than twice as often for Medicaid members.
Bonus Tip: Be sure to send text and email appointment reminders after the appointment is scheduled and follow up the appointment with digital satisfaction surveys to reinforce the importance of your members having a positive care experience.
CAHPS Measure: Getting Appointments and Care Quickly
Assuming members find the care they need, they still face overwhelming appointment wait times that diminish the member experience. Reports put the national average wait time for an appointment at 24 days.
Efficient appointment scheduling can reduce the wait time to get an appointment. ReferWell reduces that wait by about 30% or, said another way, the system books most (about 74%) of appointments within four weeks.
Action Item #5: To help members get appointments quickly, allow the plan’s in-network providers to share their schedules online and receive digital appointment bookings and requests.
Bonus Tip: Display both in-person and telehealth appointments side by side, so members can choose the most comfortable, convenient appointment location for them.
CAHPS Measure: Care Coordination
On the topic of coordinating member care and communication between providers, PCPs and specialists have, shall we say, different perceptions; 69% of PCPs reported “always” or “most of the time” sending the reason for the referral, but only 35% of specialists said they “always” or “most of the time” received clinical notes from the PCP, according to JAMA.
No matter how you interpret these results, there is ineffective communication about member care coordination.
Action Item #6: Give providers a tool to share clinical notes with specialists regardless of the various EMRs they use. Having the necessary background information in advance will save time (and prevent inconvenience) on both the provider’s and member’s sides during the specialist appointment.
Conversely, the national average for specialists closing the loop with PCPs after the appointment is just 35%. That makes it difficult to impossible for providers and plans to coordinate care and provide the appropriate follow up care to keep their members healthy.
Action Item #7: Make it easy for specialists to return consult notes and recommended follow up care using the same tool or, directly through an EMR integration.
With ReferWell, specialists close the loop 85% of the time — more than double the national average.
That also means the plan no longer needs to “chart chase” in proving that care gap closure thresholds have been met, because the plan receives documentation that the appointment occurred.
Action Item #8: Track and report on the measures that matter to your plan and use it to improve plan and provider performance.
Access reporting on the plan or provider level about member activities, specialist availability, time to appointment, provider referral behavior and more.
Your plan is undoubtedly shooting for the (4 or 5) Stars this year (#sorrynotsorry for the pun). Why not put your focus on the area where you have the greatest potential impact — those CAHPS scores that make up about a third of your Star rating?
Drilling down even further into some of the areas that have recently increased in weight — getting needed care, getting appointments and care quickly and care coordination — is going to make a significant impact on your rating. Solutions that make appointment scheduling and care coordination efficient and easy for your network providers are a great place to start moving the needle in those quadruple-the-weight areas.
Written by Paul Garrett
Paul Garrett is the former vice president of health plan sales at ReferWell.

 © COPYRIGHT REFERWELL
© COPYRIGHT REFERWELL 